Abstract
Introduction:
Heparin induced thrombocytopenia (HIT) is a well described cause of IgG antibody mediated platelet consumption.Over-testing for HIT is highly prevalent in the hospital setting. Physicians' fear of missing the diagnosis might contribute to these findings, despite the high negative predictive value of the 4T probability score and the HIT Expert Probability (HEP) score. Also, the initiation of HIT treatment pending confirmatory testing, results in a subsequent increase of costs and exposure of patients to the unnecessary risks of anticoagulation. The aim of our study is to identify clinical and laboratory factors that might affect the decision of testing for HIT in the setting of low or intermediate pretest probability and to prove that this entity is over-investigated and over-treated in the in-hospital environment.
Methods:
We conducted a cross-sectional retrospective observational study at Hofstra University Northwell Health Staten Island Hospital. Inclusion criteria were patients 18 years and older who had undergone anti-PF4-heparin antibody testing on an inpatient basis, from January 2013 till August 2015. Patients were excluded only if the test was done as outpatient. Statistical analysis was conducted using independent-sample t- test, Chi-square test or Fisher's exact test. All statistical tests were 2-sided and conducted at the 0.05 level of significance. Data was analyzed using the SAS® System Version 9.3 (SAS Institute Inc., Cary, NC).
Results:
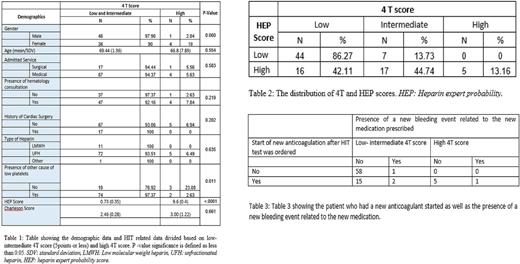
Data was collected on 89 patients who underwent anti-PF4-heparin antibody testing. 84 patients (94%) underwent HIT testing with a low 4T score, as compared to 5 patients (6%) with a high 4T score. There was no significant difference in the proportion of testing with respect to gender, age, the service under which the patient was admitted (medicine vs. surgery), presence of a hematology consult, a history of cardiac surgery, type of heparin used and an elevated Charleson score. 80% (n=74) of patients had another cause for thrombocytopenia and had the HIT panel ordered despite a low/intermediate 4T score ( Table 1).
In our study, 5 patients tested positive for HIT. 3 of the patients had high 4T and HEP score pretest probability, while 2 of the patients had intermediate 4 T score and high HEP score pretest probability. All 60 patients with a low 4 T score tested negative for HIT (Table 2).
After ordering HIT serology, heparin was discontinued in 82 patients. 17 patients with low/intermediate 4T score were started on anticoagulation, 2 of them had new bleeding event. 6 patient with high 4T score were started on anticoagulation, and 1 of them had a bleeding event (Table 3).
Conclusion:
HIT poses a significant diagnostic challenge. It is an uncommon cause of thrombocytopenia that carries significant morbidity and mortality. Our study showed that HIT testing using ELISA immunoassays is being ordered excessively in the setting of low to intermediate pretest probability leading to unwarranted treatments at significant costs and carrying an important burden on the healthcare system. However, a high number of comorbidities did not seem to lower the threshold for ordering HIT panel. It is very challenging to conduct randomized trials on less common diseases in the clinical setting to improve test ordering practices. The HEP score might be an important adjunct to clinical decision making in the future but this requires more studies being conducted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal